Income
One of the fundamental causes of health inequalities is the unequal distribution of incomes across the population.
Scottish Government data shows that in 2013-14 the
- middle 50% had just over half of all income
- top 2% had nearly 10% of all household income
- top 10% of households had around a quarter of all household income
- bottom 40% of households had around a fifth of total household income.
Individual and household incomes are influenced by a number of factors, including the tax and social security system, and the employment available.
The distribution of income between individuals and within households is influenced by a range of factors, including
- a failure to consider personal characteristics (e.g. age, gender and disability)
- how power is distributed in society
- what is seen as 'valuable' work
- dominant stories within different societies about what is fair.
This can lead to particular groups receiving lower incomes from employment and/or the state. This includes
- women
- young people
- households with a disabled person living in them.
How far these incomes stretch is affected by the cost of living.
For more information, you can read the Scottish Government’s briefing on income inequality.
How income affects health
We know that people with higher incomes are healthier. Various long term studies have established that this relationship is largely causal - higher income leads to better health.
The level and distribution of income, and poverty, is a well known cause of health inequalities within populations. It influences health directly through the goods and services that people buy which can support, or damage, their health. It also influences a wide variety of factors that have an indirect impact on health, including social status and control over unforeseen events.
However, it does not mean that those societies with the greatest incomes have the best health outcomes. The reductions in mortality seen across high income countries in the last 150 years have coincided with a prolonged period of long-run economic growth. However, the evidence that economic growth has caused improved health is actually quite weak.
For high income countries such as Scotland, it seems that socio-economic inequalities are one of the most important factors in determining overall health and the extent of health inequalities.
This means that reducing income inequality across a population is an important component of any strategy to reduce health inequalities.
Effective actions
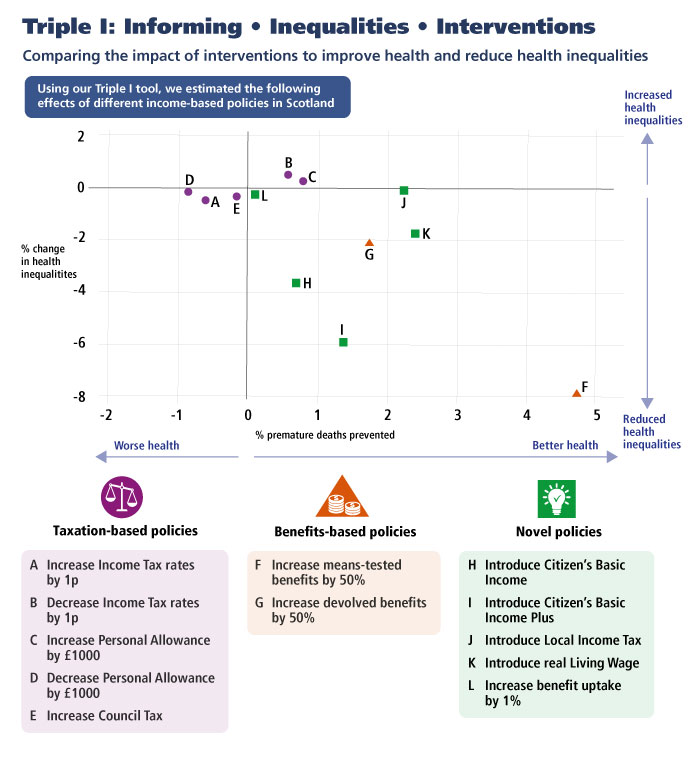
The Scottish Public Health Observatory (ScotPHO) have created the Informing Interventions to reduce health Inequalities (Triple I) tool. It estimates the likely impact of economic changes and public health interventions on health and health inequalities and can be used at a national or local level to estimate changes in deaths and hospital admissions.
ScotPHO used the tool to publish 'Income-based policies in Scotland: how would they affect health and health inequalities?' The report compares the impact of interventions on health and reducing health inequalities.
The modelling suggests that selected income-based policies could improve health and narrow health inequalities in Scotland. These policies include
- increasing means-tested benefits by 50%
- introducing illustrative Citizen's Basic Income (CBI) schemes that incorporate increases to Income Tax rates
- increasing devolved benefits by 50%
- introducing a 'real' Living Wage.
It shows the most effective income-based policies for reducing health inequalities are likely to be those that disproportionately increase incomes for those with the lowest incomes.
We have also produced a briefing on the recent discussions around a universal income policy and the implications it might have for improving health and reducing health inequalities. It links closely with NHS Health Scotland’s complementary inequality briefing on 'Income, wealth and poverty'.
We have also collaborated on a review of the impacts of universal basic income interventions, which can be accessed on the What Works Scotland site, called Universal basic income – A scoping review of evidence on impacts and study characteristics (external site).
You can also find more information on NHS Greater Glasgow and Clyde’s (NHS GGC) staff money wellbeing project. This was put in place by NHS GGC to help staff with their financial wellbeing.
How cost of living affects health inequalities
Another means of increasing the amount of money people have available is through action on the costs of living. Especially for the poorest groups, greater equity in real incomes can be achieved by reducing the cost of
- food
- transport
- childcare
- housing and the cost of heating the home.
You can find out more about how income affects health inequalities in our Income, wealth and poverty inequality briefing.
